08.02.2024 | Published by bit.bio
“Finally, the nucleus and the cell itself disintegrate and only a tangle of fibrils indicates the place where a neuron was previously located.”
– Alois Alzheimer, 19071
In looking at a magnified section of Auguste Deter’s brain, Dr. Alois Alzheimer saw a story begin to emerge. Deter, a 51-year-old woman, had been suffering from a mysterious illness that slowly eroded her cognition and drove her into bouts of rage, sadness and confusion. Deter would reach for words or names in conversation, only to find the disintegrated remains of a memory, broken and displaced by her growing dementia. In the post-mortem examination, Alzheimer could see that, gone with her memories were many of the neurons that once carried them, replaced instead by a peculiar pattern of tangled and plaque-like proteins. To Alzheimer, the source of the woman’s degenerating condition was clearly related to the appearance of these abnormal deposits1.
More than a century later, it is now understood that Deter was suffering from the first described case of Alzheimer’s disease, a neurodegenerative condition that affects roughly 45 million people worldwide2. Like Deter, patients with Alzheimer’s disease experience a progressive loss of memory and cognition that is paralleled by the death of neurons in several cortical regions of the brain. And, characteristically, this neuronal cell death is associated with rising levels of both proteinaceous neurofibrillary tangles and plaques.
For decades, these abnormal protein inclusions have been viewed as central drivers of Alzheimer’s disease pathology. However, in recent years, a new hypothesis has become apparent, one that views plaques and tangles as the potential byproducts of a much more complex and varied proteinopathy, the equivalent of embers burning in the wake of a forest fire. In the following sections, we delve into the current research on the pathology of Alzheimer’s disease and explore the ways in which protein misfolding, mislocalisation, and malfunction may lead to such ruinous outcomes.
Alzheimer's disease: a mixed proteinopathy
Alzheimer's disease is a relentless neurodegenerative disorder that progressively undermines patients' cognitive abilities, impairing their capacity to create and retrieve memories. While these symptoms are broadly observed in patients, there are many varied presentations of Alzheimer’s disease that can differ at both a molecular and clinical level. For example, in early-onset Alzheimer’s disease, patients often have mutations in key genes (such as the Amyloid Precursor Protein, APP, gene) that drive disease development much earlier in life relative to sporadic or late-onset Alzheimer’s disease3.
Like most neurodegenerative conditions, there are no clinical or macroscopic features that are truly unique to Alzheimer’s disease. Therefore, a definitive diagnosis requires pathological examination. Specifically, samples from approximately 13 different regions within the brain are assessed for the characteristic amyloid-β plaques, phosphorylated tau neurofibrillary tangles, and neuronal cell death (we will explore the makeup and significance of these in the following section). The more plaques and tangles there are, the more likely it is the patient had developed – or was in the process of developing – Alzheimer’s disease4,5.
Importantly, however, a diagnosis of Alzheimer’s disease requires the presence of both plaques and tangles – one without the other may be indicative of other neurodegenerative conditions.
A proteinopathy is any condition in which malformed or misfolded proteins are responsible – at least in part – for driving disease pathology. Proteinopathies can originate in any tissue, however the unique neuronal microenvironment appears particularly permissive. As such, many neurodegenerative diseases, including Alzheimer's disease, are also proteinopathies (Table 1).
Table 1: Proteinopathies that effect the brain
|
Proteinopathy |
Common Brain Regions Affected |
Primary Aggregating Proteins/ Peptides |
General Symptoms |
|
Alzheimer’s disease |
Hippocampus and entorhinal cortex |
Amyloid-β, tau, TDP-43 |
Memory and language impairments |
|
Parkinson’s disease |
Substantia nigra |
ɑ-synuclein |
Movement impairments: rigidity, bradykinesia, resting tremor |
|
Sporadic Creutzfeldt–Jakob disease |
Cerebral cortex and cerebellum |
Prion protein, tau |
Cognitive impairment and myoclonus |
|
Lewy body dementia |
Midbrain and neocortex |
α-synuclein, amyloid-β, Tau |
Parkinsonian syndrome, hallucinations, and sleep fluctuations |
|
Huntington’s disease |
Caudate nucleus and putamen |
Huntingtin |
Choreiform movements, bradykinesia, emotional and behavioural alterations |
|
Amyotrophic lateral sclerosis |
Motor neurons in primary cortex and spinal cord |
TDP-43, SOD |
Muscle weakness and wasting, breathing difficulties |
|
Frontotemporal dementia |
Frontal and temporal lobes |
Tau, TDP-43 |
Behavioral and emotional changes, language impairments |
Table constructed based on references 7–10
Pathological protein aggregation is often instigated by the misfolding of a protein, which may result from malformation during translation, abnormal post-translational modification (such as hyperphosphorylation), or mislocalization. Misfolded proteins tend to be sticky, meaning they are more susceptible to non-covalent bonds. The TDP-43 protein, for example, is typically expressed in the nucleus of neurons. However, in patients with frontotemporal dementia (FTD), amyotrophic lateral sclerosis (ALS), and in many individuals with Alzheimer’s disease, TDP-43 is mislocalized and hyperphosphorylated in the neuronal cytoplasm. This results in TDP-43 inclusions and subsequent neurotoxicity5–7.
Alzheimer’s disease is considered a mixed proteinopathy, meaning there are multiple malformed or misfolded proteins involved in disease pathology. In the following section, we dive into the various proteins involved in Alzheimer’s disease development and progression.
Proteins in Alzheimer's disease
As a mixed proteinopathy, much of the research on Alzheimer’s disease has focused on misfolded proteins, with a specific emphasis on amyloid-β deposits (generally referred to as plaques), and aggregates of phosphorylated tau (neurofibrillary tangles).
Amyloid precursor protein and amyloid beta
Amyloid-β is a 38 to 43 amino acid peptide that’s produced through the proteolytic cleavage of a precursor protein. Though its exact physiological role is not yet clear, evidence suggests that amyloid-β may act as a signalling molecule with downstream effects on energy metabolism throughout the body2,11. Under healthy conditions, the buildup of the peptide is unlikely due to multiple redundant control processes that stop its production or aggregation.
However, when the mechanisms that control amyloid-β levels are disrupted, self-aggregation becomes more likely. Though there are several types of amyloid-β plaque – each differing in morphology and composition – it’s believed that the process of forming these plaques is the same: soluble amyloid-β forms oligomers that encourage the formation of a sheet-like structure. These amyloid-β sheets then stack on top of one another and begin to accumulate cell debris and myriad other proteins, thus forming the basis of the quintessential plaque.
Amyloid-β plaque formation may occur years or decades before clinical symptoms of Alzheimer’s disease set in. But how – and to what extent – these plaques drive disease development is not well understood.
One potential mechanism is through the induction of excitotoxicity, wherein neurons become overstimulated through glutamate receptors. Soluble forms of amyloid-β and its oligomers may contribute to this process by prompting cells to increase the expression of glutamate receptors2,12. Another potentially indirect mechanism involves the deposition and accumulation of amyloid-β plaques in vascular tissue within the brain. When obtrusive enough, these aggregates can prevent proper blood flow, leading to hypoxic conditions and the potential death of nearby neurons5.
While certainly pathological, amyloid beta plaques themselves do not appear to be significant drivers of disease, and instead could just be a symptom. This is supported by observations of neuronal cell death in the absence of nearby plaques and the substantial lag between plaque formation and clinical symptom development.
And, while plaque formation is characteristic of Alzheimer’s disease, it’s broadly believed that amyloid-β accumulation is not in and of itself sufficient for disease development. Instead, neurodegeneration is likely a result of both amyloid-β accumulation and the rise of pathological tau species.
A tangle of tau in Alzheimer's disease
Tau is an intrinsically disordered and unfolded protein with high levels of expression in most neurons (and, to a lesser extent, in glial cells). In neurons, tau is typically concentrated along axons where it binds to and stabilizes microtubule structures, thus exerting significant influence over both axon integrity and the transport of cellular cargo to and from synapses.
Proteoforms and Tauopathies
In Alzheimer’s disease, affected neurons are likely to have a neurotoxic mix of tau species that reduce axonal transport, mediate excitotoxicity and aggregate into the mysterious neurofibrillary tangles that so captured Dr Alzheimer’s attention13,14.
Tau is a highly modifiable protein. Human tau is encoded by the MAPT gene which contains 16 exons. Alternative splicing can give rise to six different tau isoforms that differ in their affinity for microtubules and their subcellular distribution. These isoforms can be differentiated based on the number of C-terminal repeat domains they hold, with most falling into the three repeats (3R) or four repeats (4R) categories. The ratio of tau isoforms within a cell dictates axonal dynamics. An enrichment of 4R tau, which has a higher binding affinity for microtubules, may improve axonal stability, for example13,14.
Beyond alternative splicing, tau can also undergo numerous post-translational modifications, including glycosylation, ubiquitination and sumoylation, among many others, each of which may alter protein dynamics. Phosphorylation at some of the 85 potential tau phosphorylation sites, for example, is known to decrease its affinity for microtubules. As tau binding helps to stabilize the microtubule superstructure, its phosphorylation and subsequent dissociation from microtubules increase the likelihood of the structure’s collapse. This, in turn, has many downstream effects on neuronal function.
Hyperphosphorylation and enrichment of specific tau isoforms have been observed in many neurodegenerative conditions (so-called tauopathies). Progressive supranuclear palsy, Creutzfeldt–Jakob disease and argyrophilic grain disease, for example, show higher expression of 4R tau isoforms. Aggregates in Alzheimer’s disease patients are shown to contain a mixture of tau isoforms including both 4R and 3R species.
Tau's role in driving neurotoxicity in Alzheimer’s disease and other tauopathies (see Proteoforms and tauopathies section above) is a topic of ongoing investigation. However, compelling evidence points to hyperphosphorylation of tau as an important step in the neurotoxic process.
Tau has been shown to be hyperphosphorylated in Alzheimer's patients (with approximately 4-fold increase in tau phosphorylation relative to healthy adults). Phosphorylation of tau is known to decrease its affinity for microtubules which, in addition to destabilizing these structures in the neuronal axon, may increase tau’s potential to inappropriately relocate to other parts of the cell, such as dendritic spines. In relocating, tau may inadvertently concentrate some of its binding partners in aberrant locations. The protein kinase Fyn, for example, is a known binder of tau and has been implicated in amyloid-βdriven excitotoxicity. When in the postsynaptic compartment, Fyn is suspected to boost the strength of glutamate signalling by phosphorylating NMDA receptors. Therefore, relocating Fyn to the post-synaptic space may increase the strength of glutamate signalling and, with it, a neuron’s potential for excitotoxic damage13,14.
Additionally, phosphorylation encourages tau to adopt a β-sheet conformation. As with amyloid-β peptides, tau proteins that take on a β-sheet conformation are much more likely to self-aggregate into bundles. The growth of these tau bundles produces one of two superstructures: rigid and insoluble fibrils known as neurofibrillary tangles, and more flexible and structurally ambiguous tangles known as paired helical filaments – both of which originate within neurons where they have the potential to physically disrupt cellular processes.
Both neurofibrillary tangles and paired helical filaments have long been viewed as the drivers of neurodegeneration. However, there is accumulating evidence that these tau aggregates may simply be a symptom of increased pathological tau species in a cell13,14. For example, in vivo studies in mouse models of Alzheimer’s disease suggest that synapse loss, synaptic dysfunction and cognitive impairment appear before or without any eventual tangle formation. Instead, it's suspected that monomeric and oligomeric tau species may be the pathological entities14.
Such a nuanced understanding of this complex disease has not come easily. With very few tools to help make sense of Auguste Deter’s dementia, early researchers like Dr. Alzheimer assumed that the notable histological features – mostly plaques and tangles – were to blame. Researchers now have access to biorepositories, deep sequencing databases and proteomics technology (among many other tools), each of which can help untangle the disease’s pathology. To truly delve into the disease and build towards an effective therapeutic, however, researchers will need reliable in vitro disease models that provide a window into the early stages of human disease development.
Modelling Alzheimer's disease with iPSC-derived brain cells
There is much we still don’t know about the molecular pathology of Alzheimer’s disease. How, for example, do amyloid-β and phosphorylated tau drive excitotoxicity? Further, what role, if any, do neurofibrillary tangles and amyloid-β plaques play in disease pathology? And, what does this disease look like in its early stages?
To answer these questions, researchers are in need of scalable and robust models of human nerve cells. Accessing diseased neurons in living patients is prohibitively difficult. Therefore, many studies are reliant on a vanishingly small pool of patient-derived cells. Alternatively, many animal models of Alzheimer’s disease have been developed. However, these are not without their translational limitations. Adult mouse neurons, for example, typically do not express 3R tau isoforms, whereas both 3R and 4R isoforms are known to be involved in human Alzheimer’s disease13. Genetic and physiological differences like this make it difficult to study neurodegenerative processes and, in turn, greatly reduce drug development productivity.
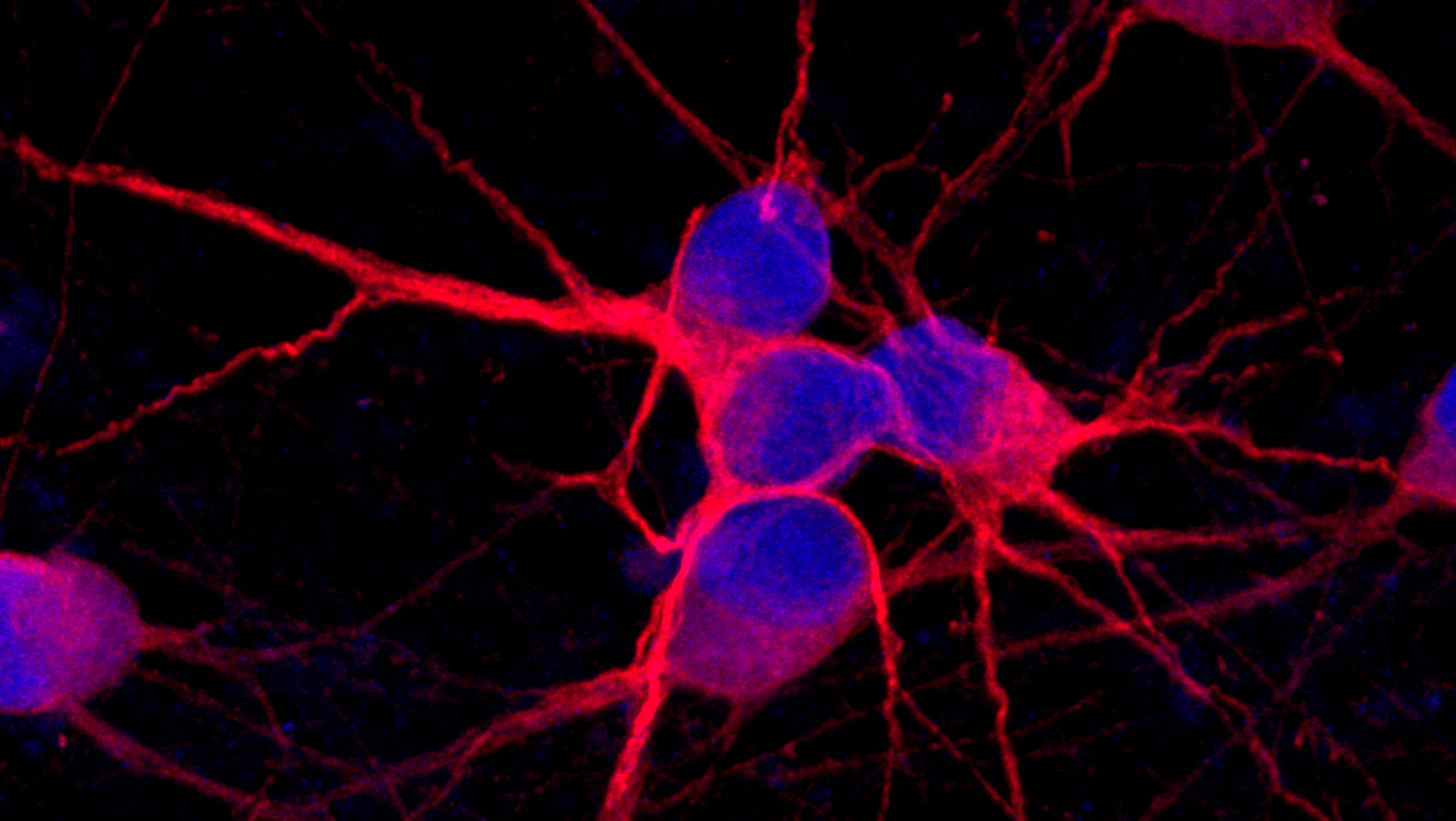
To support and accelerate Alzheimer’s disease research, bit.bio has developed human neuronal and glial cells derived from induced pluripotent stem cells, including glutamatergic, GABAergic and microglia. These cells have been engineered to include Alzheimer’s disease-relevant mutations in various genes with the goal of empowering researchers to better understand these variants, how they may contribute to disease pathology, and their potential as therapeutic targets (among many other applications). Importantly, each disease model is accompanied by its wild-type isogenic control, which allows for a uniquely well-controlled examination of each mutation’s impact on disease development and phenotypes.
bit.bio’s ioCells offer researchers a nearly infinite supply of mature human neurons and microglia, opening the door to larger-scale studies on this enigmatic disease. Click here to learn how microglia, the immune sentinels of the brain, have an emerging role in Alzheimer’s disease, and hear from Dr. Matthias Pawlowski, head of the Dementia-Sensitive Hospital at the University of Münster, who is leading several projects aimed at better understanding the pathology of Alzheimer’s disease towards developing novel therapeutic strategies.
This article is also available on Technology Networks.
References
- Alzheimer A, Stelzmann RA, Schnitzlein HN, Murtagh FR. An English translation of Alzheimer’s 1907 paper, “Uber eine eigenartige Erkankung der Hirnrinde.” Clin Anat. 1995;8(6):429-431. doi: 10.1002/ca.980080612
- Hampel H, Hardy J, Blennow K, et al. The amyloid-β pathway in Alzheimer’s disease. Mol Psychiatry. 2021;26(10):5481-5503. doi: 10.1038/s41380-021-01249-0
- McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. 2011; 7(3):263-269.9. doi: 10.1016/j.jalz.2011.03.005
- Montine TJ, Phelps CH, Beach TG, et al. National Institute on Aging–Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 2012;123(1):1-11. doi: 10.1007/s00401-011-0910-3
- DeTure MA, Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Molecular Neurodegeneration. 2019;14(1):32. doi: 10.1186/s13024-019-0333-5
- Suk TR, Rousseaux MWC. The role of TDP-43 mislocalization in amyotrophic lateral sclerosis. Molecular Neurodegeneration. 2020;15(1):45. doi: 10.1186/s13024-020-00397-1
- Noor A, Zafar S, Zerr I. Neurodegenerative proteinopathies in the proteoform spectrum—tools and challenges. Int J Mol Sci. 2021;22(3):1085. doi: 10.3390/ijms22031085
- Guo W, Fumagalli L, Prior R, Van Den Bosch L. Current advances and limitations in modeling ALS/FTD in a dish using induced pluripotent stem cells. Front Neurosci. 2017;11:671. doi: 10.3389/fnins.2017.00671
- Frontotemporal dementia vs. ALS. ALS Therapy Development Institute. Published April 14, 2021. Accessed February 5, 2024. https://www.als.net/news/frontotemporal-dementia-vs-als/
- Virgilio E, De Marchi F, Contaldi E, et al. The role of tau beyond Alzheimer’s disease: a narrative review. Biomedicines. 2022;10(4):760. doi: 10.3390/biomedicines10040760
- Shigemori K, Nomura S, Umeda T, Takeda S, Tomiyama T. Peripheral Aβ acts as a negative modulator of insulin secretion. Proc Natl Acad Sci USA. 2022;119(12):e2117723119. doi: 10.1073/pnas.2117723119
- Dong X xia, Wang Y, Qin Z hong. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol Sin. 2009;30(4):379-387. doi: 10.1038/aps.2009.24
- Wang Y, Mandelkow E. Tau in physiology and pathology. Nat Rev Neurosci. 2016;17(1):22-35. doi: 10.1038/nrn.2015.1
- Hyman B. All the tau we cannot see. Annu Rev Med. 2023;74(1):503-514. doi: 10.1146/annurev-med-042921-02374