29.11.2023 | Published by bit.bio
For much of his career, Professor Ludovic Vallier has focused his research on how the human liver develops and regenerates. This vital organ serves myriad functions in the human body, including a critical role in defending us from toxic chemicals. However, every year, millions of people around the world die as a result of liver failure1. Yet, for all of its importance, studying the development and decline of this organ remains a considerable challenge, one that hinders drug development and patient care.
Professor Vallier, a professor of Stem Cells in Regenerative Therapies at the Berlin Institute of Health and a Max Plank Fellow at Max Planck Institute for Molecular Genetics, is working to change this. For the past 20 years, Professor Vallier has been working on generating functional hepatocytes in vitro for clinical applications, including disease modelling and cell-based therapy2.
In the sections that follow, we’ll explore the importance of hepatocytes, their role in the body and the potential they have as a cell-based therapy.
What are hepatocytes?
Hepatocytes are the predominant cell type of our largest internal organ, the liver, comprising 90% of its mass. With 80–100 billion hepatocytes per human liver, this makes it one of the most abundant cell types in the body.
What do hepatocytes do?
Hepatocytes have an extraordinarily broad range of functions. They play a key role in detoxification of the blood, eliminating ammonia from the body via the urea cycle, and metabolising alcohol, drugs and other toxins with cytochrome P450 enzymes, particularly CYP3A4, which is responsible for metabolising 40–50% of all clinically relevant drugs. They are also crucial for glucose homeostasis, acting as a reservoir to store glycogen and maintain a healthy blood sugar level. They regulate lipid uptake and release, controlling arterial lipid levels, and they contribute to bile production to emulsify fats in the diet. They secrete many of the body’s proteins, most importantly clotting factors and albumin. In addition, they are a key cell type for the production and storage of iron and vitamins.
With such versatile functions, it’s not surprising that researchers such as Vallier are interested in studying hepatocytes for a wide range of applications, including preclinical toxicology and the development of novel cell therapies.
Watch this short video with Vallier to hear his thoughts on the need for, and importance of, novel treatments for patients with liver diseases and how hepatocyte-based therapies could play a role.
How do hepatocytes carry out their specialised functions?
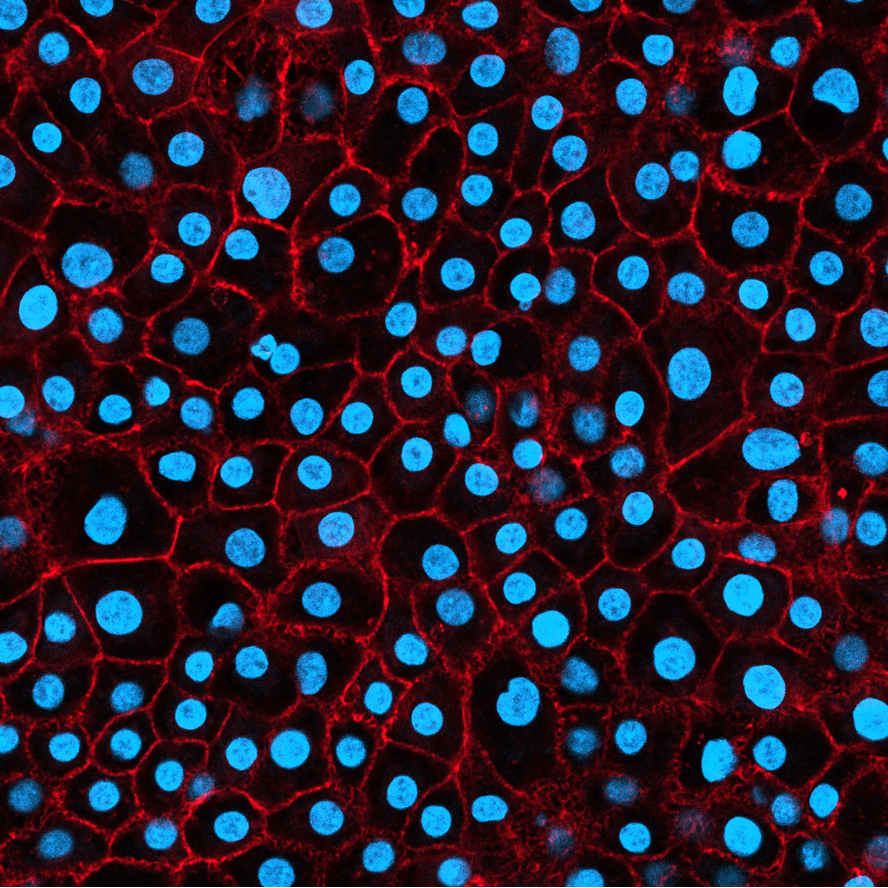
Hepatocytes’ multi-functionality is acquired during their differentiation from hepatoblasts, which is dependent on signalling gradients provided by the microenvironment during foetal development. Hepatocytes are often polyploid and binucleated, with plentiful smooth endoplasmic reticulum and free ribosomes, characteristics which underpin their complex and prolific secretory system. Numerous mitochondria deliver the high energy requirements of their multiple metabolic pathways. Their cellular architecture is cuboidal, and their arrangement in the liver parenchyma is highly precise; hepatocytes are organised into lobules representing the basic functional unit, connected with the biliary, artery and venous system to efficiently filter blood.
The liver is unique among the human organs in having a highly regenerative capacity. This fact was known to the ancient Greeks and promulgated via the legend of Prometheus, whose liver regrew each night despite being pecked out by an eagle each day. After acute injury involving loss of two thirds of the liver, the organ can regrow back to its original size and functionality. However, some chronic liver diseases target this regenerative capacity by inhibiting hepatocyte proliferation and rendering the liver incapable of regrowth.
Which diseases could we address if we had a greater understanding of hepatocytes?
Hepatocytes are implicated in many serious health conditions. Acute physical injury, toxic overdose or viral infection can cause acute liver failure. Chronic liver diseases can result in inflammation (hepatitis), fat accumulation (steatosis), or severe permanent scarring (cirrhosis).
“Liver disease is growing as a challenge worldwide”, says Professor Vallier, “and at present, the only treatment for end-stage liver disease is liver transplantation. This is extremely complicated; we don’t have enough organ donors, the surgery is very dangerous, and then patients need immunosuppression, which affects quality of life and reduces life expectancy. To establish hepatic function and preserve life, we need 1–5% of functional hepatocytes, which is roughly equivalent to 1–5 billion cells per patient.”
Professor Vallier studies liver diseases, especially non-alcoholic fatty liver disease (NAFLD)3. This increasingly prevalent chronic condition affects over 30% of the population, and risk is sharply elevated by diabetes and obesity. Therapies using hepatocytes to rebuild the damaged liver offer great potential. Unfortunately, donated primary hepatocytes are in short supply, and, in vitro, they de-differentiate extremely quickly.
How scientists study hepatocytes: From primary human hepatocytes to iPSC-derived cells
For many years, rat hepatocytes were a popular source of cells because it is feasible — albeit expensive and ethically complicated — to grow and harvest liver tissue from rats. While accessible, the pharmacological relevance of rat hepatocytes is severely limited by genetic differences between rats and humans, greatly reducing their predictive power for human hepatocyte behaviour4. One option is to collect hepatocytes from a human liver. These primary human hepatocytes are often mature, differentiated cells that retain some of their in vivo behaviour. As such, they can be a good proxy for the human liver.
However, in their 2022 publication5, Vallier and his coauthors described the challenges of working with primary hepatocytes, specifically stating that “primary human hepatocytes are in short supply as they can only be obtained from suboptimal livers unsuitable for transplantation.” The team also highlighted that these cells “display a short life, [an] absence of proliferation, and rapid loss of functionality in vitro.”
Compounding these issues is the genetic variation that can exist between donors, which can lead to discordant results between studies. In short, primary human hepatocytes are not able to meet the field’s needs.
The future for therapies and further applications
Professor Vallier’s goal is to develop new cell-based therapies using forward programming to create hepatocytes from pluripotent stem cells via overexpression of transcription factors5,6. Specifically, in 2022, Vallier and his colleagues had a breakthrough by leveraging bit.bio’s optimised inducible overexpression (opti-ox) technology which enables the precise reprogramming of human iPSCs to desired cell types5. Vallier and his team used opti-ox to produce a population of hepatocytes that, according to Vallier, “express homogeneously key hepatocyte markers and display key hepatic functions.”
At bit.bio, we are also using induced hepatocyte-like cells - we call them txHepatocytes - in our lead cell therapy candidate: bbHEP01.
bbHEP01 is in development as a treatment for patients suffering from acute liver failure (ALF) and acute-on-chronic liver failure (ACLF), considered life-threatening liver conditions with high mortality. bbHEP01 consists of encapsulated allogeneic txHepatocytes produced with opti-ox. The product is designed to provide transient liver function support, allowing native liver recovery or providing a bridge to transplant. This approach builds on current preclinical and clinical data demonstrating the feasibility and potential benefit of encapsulated donor-derived hepatocyte cell therapy17-11.
A deeper understanding of hepatocytes would not only revolutionise medicine for chronic and acute liver diseases, but also improve toxicity screening of these medicines. As key cells for detoxification, hepatocytes are very sensitive to toxins. “Testing of drug toxicity by pharma companies is currently done via rat hepatocyte tox-screen”, says Vallier. “Often, the drug gets withdrawn only when it fails in humans, because the toxicity profile doesn’t translate across species. If we could generate human hepatocytes robustly in vitro, we could improve and refine the safety profile of drugs.”
Watch this short video to hear Vallier discuss the use of liver cells in drug toxicology.
Human hepatocytes will be pivotal for modelling human diseases. “If we could build a panel of functional hepatocytes with different genetics12, such as different gender or ethnicity, we could better understand the risk factors for fatty liver disease. Access to functional hepatocytes would allow us to model diseases such as NAFLD without having to rely on animal models”, says Professor Vallier.
Just as the mythical Prometheus’ liver generated a never-ending supply of hepatocytes, precision cellular reprogramming may provide an infinite source of human hepatocytes in vitro, for use as therapies and across the whole drug development process.
References
- Asrani, Sumeet K., et al. (2019) Burden of Liver Diseases in the World. Journal of Hepatology 70(1): 151-171. https://doi.org/10.1016/j.jhep.2018.09.014
- Yiangou L, Ross ADB, Goh KJ, Vallier L (2018) Human pluripotent stem cell-derived endoderm for modeling development and clinical applications. Cell Stem Cell 22(4): 485-499. https://doi.org/10.1016/j.stem.2018.03.016
- Tilson SG, Morell CM, Lenaerts A-S, Park SB, Hu Z, Jenkins B, Koulman A, Liang TJ, Vallier L (2021) Modeling PNPLA3-associated NAFLD using human-induced pluripotent stem cells. Hepatology 74: 2998-3017. https://doi.org/10.1002/hep.32063
- Martignoni, Marcella, et al. (2006) Species Differences between Mouse, Rat, Dog, Monkey and Human CYP-Mediated Drug Metabolism, Inhibition and Induction. Expert Opinion on Drug Metabolism & Toxicology 2(6): 875-894. https://doi.org/10.1517/17425255.2.6.875
- Tomaz RA, Zacharis ED, Bachinger F, Wurmser A, Yamamoto D, Petrus-Reurer S, Morell CM, Dziedzicka D, Wesley BT, Geti I, Segeritz C-P, de Brito MC, Chhatriwala M, Ortmann D, Saeb-Parsy K, Vallier L (Preprint, 26 June 2022) Generation of functional hepatocytes by forward programming with nuclear receptors. https://doi.org/10.1101/2022.06.23.497371
- Wesley BT, Ross ADB, Muraro D, Miao Z, Saxton S, Tomaz RA, Morell CM, Ridley K, Zacharis ED, Petrus-Reurer S, Kraiczy J, Mahbubani KT, Brown S, Garcia-Bernardo J, Alsinet C, Gaffney D, Tysoe OC, Botting RA, Stephenson E, Popescu D-M, MacParland S, Bader G, McGilvray ID, Ortmann D, Sampaziotis F, Saeb-Parsy K, Haniffa M, Stevens KR, Zilbauer M, Teichmann SA, Vallier L (Preprint, 09 March 2022) Single-cell atlas of human liver development reveals pathways directing hepatic cell fates. https://doi.org/10.1101/2022.03.08.482299
- Dhawan et al. Alginate microencapsulated human hepatocytes for the treatment of acute liver failure in children. J Hepatology 2020;72: 877-884. https://pubmed.ncbi.nlm.nih.gov/31843649/
- Mai G, Nguyen T, Morel P, Mei J, Andres A, Bosco D, et al. Treatment of fulminant liver failure by transplantation of microencapsulated primary or immortalized xenogeneic hepatocytes. Xenotransplantation 2005;12:457–464. https://pubmed.ncbi.nlm.nih.gov/16202069/
- Mei J, Sgroi A, Mai G, Baertschiger R, Gonelle-Gispert C, Serre-Beinier V, et al. Improved survival of fulminant liver failure by transplantation of microencapsulated cryopreserved porcine hepatocytes in mice. Cell Transplant 2009;18:101–110. https://pubmed.ncbi.nlm.nih.gov/19476213/
- Sgroi A, Mai G, Morel P, Baertschiger R, Gonelle-Gispert C, Serre-Beinier V, et al. Transplantation of encapsulated hepatocytes during acute liver failure improves survival without stimulating native liver regeneration. Cell Transplant 2011;20:1791–1803. https://pubmed.ncbi.nlm.nih.gov/21396154/
- Umehara Y, Hakamada K, Seino K, Aoki K, Toyoki Y, Sasaki M. Improved survival and ammonia metabolism by intraperitoneal transplantation of microencapsulated hepatocytes in totally hepatectomized rats. Surgery 2001;130:513–520. https://pubmed.ncbi.nlm.nih.gov/11562677
- Segeritz C-P, Rashid ST, de Brito MC, Serra MP, Ordonez A, Morell CM, Kaserman JE, Madrigal P, Hannan NRF, Gatto L, Tan L, Wilson AA, Lilley K, Marciniak SJ, Gooptu B, Lomas DA, Vallier L (2018) hiPSC hepatocyte model demonstrates the role of unfolded protein response and inflammatory networks in α1-antitrypsin deficiency. Journal of Hepatology 69 (4): 851-860. https://doi.org/10.1016/j.jhep.2018.05.028